No products in the cart.

Stretcher Pads in the Emergency Department: Better Support Surfaces, Better Patient Outcomes
By prioritizing patient care and providing appropriate support surfaces, healthcare facilities can improve patient outcomes. The Emergency Department (ED) is the primary point of entry to the acute health care system. Unfortunately, patients too often leave the ED with painful pressure ulcers that could have been avoided, especially elderly individuals with multiple pre-existing conditions, which is why high-quality stretcher pads in the emergency department are crucial.
Even though skin protection is a low priority in life-threatening situations, preventive measures should be implemented once the patient’s condition has stabilized. The likelihood of patients developing pressure ulcers can decrease exponentially when clinicians provide appropriate support surfaces for their risk level. By looking at risk factors for pressure injury development in the ED and interventions to protect patients’ skin, health systems can improve patient outcomes and reduce unnecessary expenses.
Risk Factors
Arrival to the ED via ambulance is a significant risk factor for pressure injury development due to acute injury and immobilization on spinal boards. These patients are also more likely to be older and more acutely ill with impaired circulation. Skin breakdown can even develop en route to the ED when frail patients are secured to relatively hard, narrow ambulance stretchers (2). Staying in the ED for more than four hours is an independent risk factor for pressure injury development as well (3). The average ED stay is more than eight hours and can be greater than 24 hours for patients who are waiting for an inpatient bed (4).
Assessment in the ED
Best practice guidelines recommend performing skin assessments as soon as possible to identify pressure ulcers that are present on arrival. This enables prompt implementation of skin protection protocols and ensures that pre-existing wounds are not inadvertently categorized as hospital-acquired (2). While the Braden scale is commonly used for hospitalized patients, the shorter PURPOSE-T and Norton pressure ulcer risk assessment tools are better suited for the ED (5, 6, 7). Elevated C-reactive protein (CRP) level and fever are additional independent risk factors for skin breakdown that must also be considered (5).
Prevention
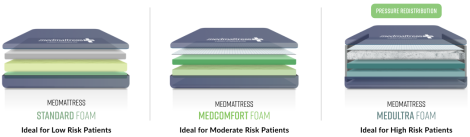
Immobilization devices such as cervical collars and backboard should be removed as soon as spinal injury has been ruled out. When performing skin assessments, providers should always check for catheters, wires, IV tubing or discarded needle covers that may be underneath the patient. These can quickly cause localized device-related pressure ulcers that can take months to heal. Repositioning schedules should be instituted as soon as possible and the skin should be protected from urine, feces, or other fluids (5). Patients at high risk for skin breakdown should be placed on stretchers with pressure redistribution mattresses upon arrival at the ED (8). These stretcher mattresses feature multiple layers of high density foam that are much more protective than standard stretcher pads. The soft conforming foam layer immerses the patient’s body to protect bony prominences and maintain circulation. The top layer of cool gel memory foam allows continuous airflow to keep the patient’s skin cool and dry. MedMattress Stretcher Pads are available in three foam qualities: Standard Foam, MedComfort Foam and MedUltra Foam.
Conclusion
Pressure ulcers are one of the most common complications in the ED, especially in patients who are immobile, elderly or seriously ill. The Norton and PURPOSE-T assessment tools allow providers to quickly identify patients who are at risk of developing skin breakdown. Removing immobilization devices as soon as possible, repositioning schedules and meticulous skin care can help prevent pressure ulcers from developing. High risk patients should also be placed on stretchers with pressure redistribution mattresses rather than standard pads to avoid developing pressure injuries.
MedMattress Stretcher Pads are available in three foam levels depending on the patient’s assigned risk level. MedMattress Standard Foam Stretcher Pads are ideal for low risk patients, MedComfort Foam is best suited for moderate risk patients and MedUltra Foam features advanced pressure redistribution for high risk patients. For your convenience, shop by stretcher manufacturer or model and then select your preferred foam quality.
References
- Liu, P., Shen, W., & Chen, H. (2017). The incidence of pressure ulcers in the emergency department: A meta-analysis. Index Wounds, 29(1), 14-19.
- Fulbrook, P., Miles, S., & Coyer, F. (2019). Prevalence of pressure injury in adults presenting to the emergency department by ambulance. Australian Critical Care, 32(6), 509-514.
- Han, D., Kang, B., Kim, J., Jo, Y., … Jang, D. (2020). Prolonged stay in the emergency department is an independent risk factor for hospital‐acquired pressure ulcers. International Wound Journal,17(2), 259–267.
- Dugaret, E., Videau, M., Faure, I., Gabinski, C., … Salles, N. (2014). Prevalence and incidence rates of pressure ulcers in an Emergency Department. International Wound Journal, 11(4), 386-391.
- Santamaria, N., Creehan, S., Fletcher, J., Alves, P., & Gefen, A. (2019). Preventing pressure injuries in the emergency department: Current evidence and practice considerations. International Wound Journal, 16(3), 746-752.
- Coleman, S., Smith, I., McGinnis, E., Keen, J., … Nixon, J. (2018). Clinical evaluation of a new pressure ulcer risk assessment instrument, the Pressure Ulcer Risk Primary or Secondary Evaluation Tool (PURPOSE T). Journal of Advanced Nursing, 74(2), 407–424.
- Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals. Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu7b.html
- Long, D. (2018). Best practices for pressure injury prevention in the ED. Retrieved from https://americannursetoday.mydigitalpublication.com/publication/?m=41491&i=492685&view=articleBrowser&article_id=3075007&ver=html5
You might also be interested in:

-
/
Rest for Success: When to Bid Adieu to Your Old Mattress
Rest for Success: When to Bid Adieu to Your Old Mattress We spend about a third of our lives in bed, and the quality of our sleep directly impacts our overall well-being. One often overlooked factor in achieving a good night’s sleep is the condition of our mattress. As the years go by, our faithful […]
Read more
Unveiling the Truth: Busting Common Mattress Myths
Unveiling the Truth: Busting Common Mattress Myths A good night’s sleep is crucial for overall well-being, and the right mattress plays a pivotal role in achieving that. However, amidst the quest for the perfect mattress, numerous misconceptions have caused mattress shoppers confusion when searching for the right mattress. Our latest blog unravels the truth behind […]
Read more
-
/
How Medical Bed Mattresses Aid in Post-Surgery Recovery
How Medical Bed Mattresses Aid in Post-Surgery Recovery Surgery can be a daunting experience, regardless of its nature or severity. The period following a surgical procedure, known as post-surgery recovery, is crucial for achieving the best possible outcome. While factors like rest, nutrition and pain management are widely acknowledged as vital, the role that medical […]
Read more
-
/
Meeting Medical Mattress Quality Standards
Meeting Medical Mattress Quality Standards Medical mattresses are designed to meet specific quality standards to ensure patient safety, comfort and hygiene. These standards are established to address the unique needs of healthcare environments as well as the patients utilizing these mattresses. Some key quality standards for medical mattresses include: Infection Control Standards Water […]
Read more