No products in the cart.

Better Support Surfaces, Better Patient Outcomes
At MedMattress, we believe that better support surfaces produce better patient outcomes. By providing our customers with quality support surfaces designed for the needs of every patient, we can help improve the quality of healthcare.
Decubitus ulcers are the leading complication in healthcare facilities across the U.S., costing up to $26 billion and resulting in more than 60,000 patient deaths each year (1, 2). More than half of patients who are hospitalized with decubitus ulcers die during the next 12 months (2). Prevention of decubitus ulcers must be an all-important safety goal for all areas of healthcare to protect patients from this avoidable complication. Clinicians can prioritize patient safety and positive outcomes by accurately predicting the risk for each patient and providing therapeutic support surfaces for patients at moderate or high risk for skin breakdown (3, 4).
What are Decubitus Ulcers?
Decubitus ulcers, or pressure sores, occur when a patient lays in one position for extended periods of time with little or no movement, causing damage to the skin and underlying tissues. The heels, hips, ankles, and tailbone are considered high risk areas and are most susceptible to pressure injury which can cause significant tissue damage in just a few hours. Treatment of decubitus ulcers requires a comprehensive approach including frequent and meticulous wound care, debridement, pain management and infection prevention (5).
Decubitus Ulcer Risk Assessment
Patients who are bedridden, unconscious, immobile or unable to sense pain are at higher risk for developing decubitus ulcers. Diabetes, impaired circulation and malnutrition also increase the risk of skin breakdown. The Braden Scale has been used for more than two decades to identify and quantify risk for developing pressure ulcers based on six areas: Sensory Perception, Moisture, Activity, Mobility, Nutrition and Friction/Shear (6). The goal of the Braden Scale is to accurately identify which patients are at high risk who require aggressive preventive care and to screen out those who are at lower risk. Research has shown the Braden Scale to be a reliable instrument for acute and long term care, especially for identifying risk factors related to sensory perception and friction (7).
Braden Scale Scoring
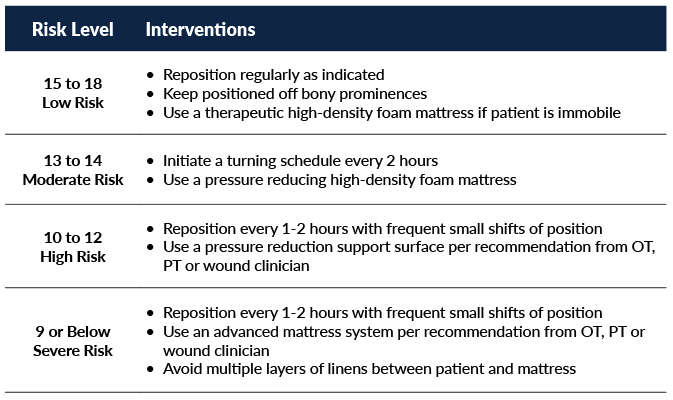
Each area of the Braden Scale is scored to present an overall risk assessment on a scale of 6 to 20. Patients at highest risk for pressure injuries have the lowest scores on the Braden Scale (8).
While interventions to prevent skin breakdown are individualized for each patient, general recommendations include:
How Therapeutic Support Surfaces Work
Pressure-relieving support surfaces redistribute the patient’s body weight over a large surface area to relieve pressure on high risk areas and bony prominences (9). Therapeutic support surfaces help maintain blood flow to at-risk areas and can help reduce the incidence of pressure injuries by up to 60% (9). They use immersion to redistribute pressure over the patient’s entire body, not just the bony prominences (10). As the patient sinks down, more of the patient’s body comes into contact with the support surface, so that the patient’s weight is spread over a larger area (11). Greater contact between the body surface and the mattress results in decreased pressure and decubitus ulcer risk. Because warm, moist skin is a risk factor for pressure injuries, some therapeutic support surfaces maintain air flow to keep the skin cool and wick moisture away.
Types of Therapeutic Support Surfaces
Foam is the most commonly used support surface with many types of layers, zones, densities and features to choose from (10). A softer foam is recommended to cradle the head and heels while higher density foam is placed around the edges of the mattress for side support. More advanced mattress systems with low air loss, zero interface pressure, alternating pressure and lateral rotation are needed for patients at highest risk for skin breakdown or to treat existing decubitus ulcers. Reactive support surfaces like multi-density, multi-layer foam mattresses change pressure distribution when the patient lays or sits on them (11). Active support surfaces are powered systems that include alternating pressure and low air loss mattresses (12).
Choosing Therapeutic Support Surfaces
A comprehensive assessment is required to determine which type of therapeutic support surface is best suited to meet the patient’s needs (9). Important factors for decision making include but are not limited to:
- Advanced age
- Nutritional status
- Hemodynamic stability
- Presence of edema
- Patient’s weight
- Presence of fever
- History of pressure ulcers
- Present skin condition
- Presence of anemia
Active and reactive support surfaces have been shown to reduce the risk of pressure ulcers as compared with standard mattresses and should be used for patients at high risk of skin breakdown. Multi-density, multi-layer foam mattresses are recommended for patients with limited mobility while alternating pressure and low air loss mattresses should be used for patients who are immobile. Consultation with therapists and wound care clinicians is helpful for determining which therapeutic support surface is most appropriate for patients (9).
Specialty Areas
The need for therapeutic support surfaces extends beyond inpatient units in acute care settings. Pressure ulcers can develop in as little as 2 hours while patients lay on stretchers for prolonged periods of time in the emergency department (ED), especially when admission to inpatient units is delayed due to high patient census (13,14). Immobilization on hard surfaces such as backboards and scan tables is often required as injuries are assessed, preventing repositioning or ambulation. Shear injuries to the skin occur as patients attempt to shift their weight while immobilized. Elderly patients or those with multiple comorbidities, poor nutritional status and elevated C-reactive protein (CRP) levels are at highest risk for developing decubitus ulcers in the ED (14, 15). The PURPOSE T pressure ulcer risk assessment tool is designed specifically for use in the ED so that clinicians can implement skin protection protocols including multi-layered pressure redistribution foam stretcher pads (15, 16).
The operating room is another area where patients commonly develop pressure ulcers, especially during surgical procedures that last longer than three hours (17, 18). General anesthesia, use of tourniquets, low body temperature and supine positioning are additional risk factors for pressure ulcers that are specific to the surgical area (19). Research has shown that pressure redistributing foam mattresses and positioning devices with air or gel pad overlays can significantly reduce the risk of skin breakdown as compared to standard 2” foam pads (17, 18). Mattress covers must provide excellent infection control features as well as fire retardant properties (20). Appropriate padding is needed between the patient and surgical equipment such as stirrups and extremity holders as pillows and molded foam devices may not be sufficient to prevent skin breakdown (20).
Conclusion
MedMattress therapeutic support surfaces can help protect patients from developing painful pressure ulcers by redistributing pressure, reducing shearing forces and controlling the local microclimate. Clinicians and caregivers’ pressure injury prevention protocols should include careful selection of appropriate support surfaces in addition to risk assessment tools, repositioning schedules and meticulous skin care. Our entire collection of MedMattress medical support surfaces are designed to be simple for clinicians to select the appropriate mattress or surface for their patients needs.
The MedMattress Care Collection offers a selection of hospital bed mattresses for every level of care. Our Care Med-Surg Mattresses are designed to target a specific patient risk level from low risk to high risk.
MedMattress offers standard Foam, MedComfort Foam and MedUltra Pressure Redistribution Foam for any replacement stretcher pad or gurney mattress. Our replacement gurney pads and stretcher mattresses provide solutions for a variety of clinical and budget needs. When selecting which replacement stretcher pad is right for your facility, keep in mind that patients are moved throughout the hospital frequently which means the stretcher pad needs to combine both comfort and durability.
We also offer a dedicated line of Operating Room Table Pads and Surgical Surfaces designed with patient care in mind. Available in three (3) foam qualities to target the specific needs of any patient, MedMattress Surgical Table Pads provide advanced pressure redistribution for high risk patients or elevated comfort and support for low risk patients.
References
- Morse, S. (2019). Pressure ulcers cost the health system $26.8 billion a year. Retrieved from https://www.healthcarefinancenews.com/news/pressure-ulcers-cost-health-system-268-billion-year
- Kirman, C. (2020). What is the mortality rate for pressure injuries (pressure ulcers)? Retrieved from https://www.medscape.com/answers/190115-82434/what-is-the-mortality-rate-for-pressure-injuries-pressure-ulcers
- Nursing Times. (2012). Pressure ulcer risk assessment. Retrieved from https://www.nursingtimes.net/clinical-archive/tissue-viability/pressure-ulcer-risk-assessment-20-01-2012/
- Shi, C., Dumville, J., & Cullum, N. (2018). Support surfaces for pressure ulcer prevention: A network meta-analysis. PLoS One, 13(2), e0192707.
- Gould, L., Bohn, G., Bryant, R., Paine, T., …Simman, R. (2019). Pressure ulcer summit 2018: An interdisciplinary approach to improve our understanding of the risk of pressure-induced tissue damage. Wound Repair and Regeneration, 27(5), 497-508.
- Huang, C., Ma, Y, Wang, C., Jiang, M., … Han, L. (2021). Predictive validity of the braden scale for pressure injury risk assessment in adults: A systematic review and meta-analysis. Nursing Open, 8(5), 2194-2207.
- Kring, D. (2007). Reliability and validity of the Braden Scale for predicting pressure ulcer risk. Journal of Wound, Ostomy and Continence Nursing, 34(4), 399-406.
- Advances in Skin & Wound Care. (2004). By the numbers: Braden score interventions.17(3), 150.
- McNicol, L., Mackey, D., Watts, C., & Zuecca, N. (2020). Choosing a support surface for pressure injury prevention and treatment. Nursing 2021, 50(2), 41-44.
- Sidor, D., & Sieggreen, M. (2018). Navigating the maze of support surfaces. Retrieved from https://www.myamericannurse.com/wp-content/uploads/2018/05/ANT0518_Dabir_NavigatingMazeSupportSurfaces.pdf
- Ovens, L. (2017). How to guide: Selecting a support surface. Retrieved from https://www.woundsinternational.com/resources/details/how-to-guide-selecting-a-support-surface
- Haesler, E. (2018). Pressure injuries: Active support surfaces for preventing and treating pressure injuries. Wound Practice and Research, 26(1), 50-51.
- Liu, P., Shen, W., & Chen, H. (2017). The incidence of pressure ulcers in the emergency department: A meta-analysis. Index Wounds, 29(1), 14-19.
- Dugaret, E., Videau, M., Faure, I., Gabinski, C., … Salles, N. (2014). Prevalence and incidence rates of pressure ulcers in an Emergency Department. International Wound Journal, 11(4), 386-391.
- Santamaria, N., Creehan, S., Fletcher, J., Alves, P., & Gefen, A. (2019). Preventing pressure injuries in the emergency department: Current evidence and practice considerations. International Wound Journal, 16(3), 746-752.
- Coleman, S., Smith, I., McGinnis, E., Keen, J., … Nixon, J. (2018). Clinical evaluation of a new pressure ulcer risk assessment instrument, the Pressure Ulcer Risk Primary or Secondary Evaluation Tool (PURPOSE T). Journal of Advanced Nursing, 74(2), 407–424.
- Primiano, M., Friend, M., McClure, C., Nardi, S., … Savochka, K. (2011). Pressure ulcer prevalence and risk factors among prolonged surgical procedures in the OR. AORN, 94(6), 555-566.
- Oliveira, K., Pires, P., De-Mattia, A., Barichello, E., … Barbosa, M. (2018). Influence of support surfaces on the distribution of body interface pressure in surgical positioning. Revista Latino-Americana de Enfermagem, 26, e3083.
- Aronovich, S. (2007). Intraoperatively acquired pressure ulcers: Are there common risk factors? Ostomy and Wound Management, 53(2), 57-69.
- Fawcett, D., Black, J., & Scott, S. (2014). Ten top tips: Preventing pressure ulcers in the surgical patient. Retrieved from https://www.woundsinternational.com/resources/details/ten-top-tips-preventing-pressure-ulcers-in-the-surgical-patient
You might also be interested in:

-
/
Rest for Success: When to Bid Adieu to Your Old Mattress
Rest for Success: When to Bid Adieu to Your Old Mattress We spend about a third of our lives in bed, and the quality of our sleep directly impacts our overall well-being. One often overlooked factor in achieving a good night’s sleep is the condition of our mattress. As the years go by, our faithful […]
Read more
Unveiling the Truth: Busting Common Mattress Myths
Unveiling the Truth: Busting Common Mattress Myths A good night’s sleep is crucial for overall well-being, and the right mattress plays a pivotal role in achieving that. However, amidst the quest for the perfect mattress, numerous misconceptions have caused mattress shoppers confusion when searching for the right mattress. Our latest blog unravels the truth behind […]
Read more
-
/
How Medical Bed Mattresses Aid in Post-Surgery Recovery
How Medical Bed Mattresses Aid in Post-Surgery Recovery Surgery can be a daunting experience, regardless of its nature or severity. The period following a surgical procedure, known as post-surgery recovery, is crucial for achieving the best possible outcome. While factors like rest, nutrition and pain management are widely acknowledged as vital, the role that medical […]
Read more
-
/
Meeting Medical Mattress Quality Standards
Meeting Medical Mattress Quality Standards Medical mattresses are designed to meet specific quality standards to ensure patient safety, comfort and hygiene. These standards are established to address the unique needs of healthcare environments as well as the patients utilizing these mattresses. Some key quality standards for medical mattresses include: Infection Control Standards Water […]
Read more